Specialty pharmacy medications are a vital component of treatment for some of the most complex (and oftentimes rare) conditions, including cancers, autoimmune conditions and genetic disorders.
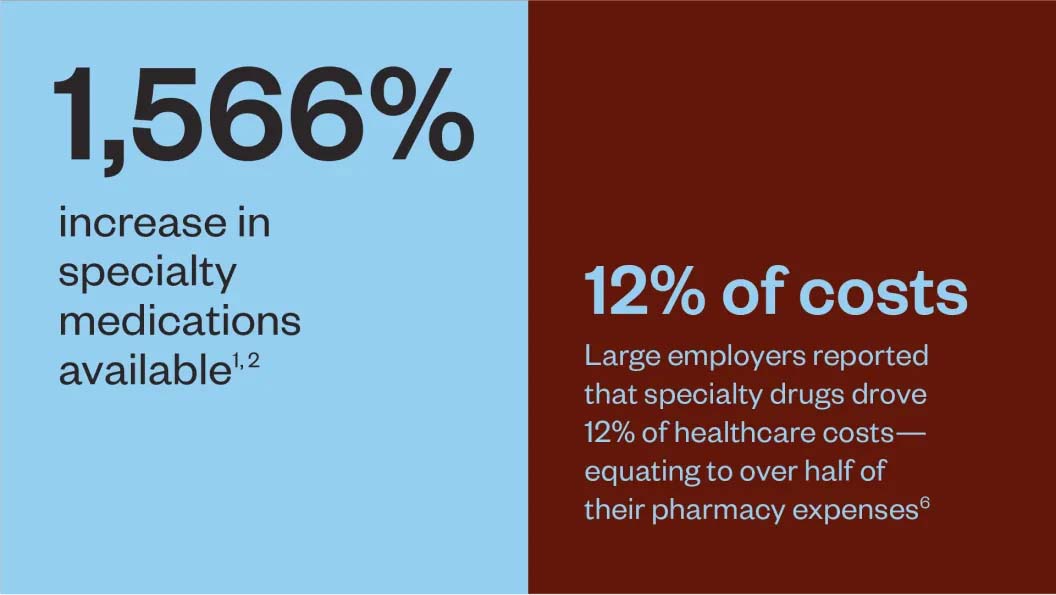
In the early 1990s, specialty pharmacy options were limited, with fewer than 30 medications approved for use by the U.S. Food and Drug Administration.1 Fast forward to today, and there are more than 1,000 specialty pharmacy drugs available on the market, with hundreds more in various stages of development and around 50 approved just last year.2
Contributing to this massive growth are advances in healthcare (medicines, as well as other treatments) that have led to fewer people dying from complex conditions. For example, the cancer mortality rate has declined over the last 30 years by 39%,3 despite an overall rise in cancer incidence, with 2024 marking the first year where new cases are predicted to surpass the 2-million mark.4
These medications, which have advanced rapidly in recent years, have dramatically increased in cost, and it’s estimated that specialty medicines will represent 43% of global spending in 2027.5 Without proactive intervention, these rising costs will continue to pose significant financial burdens on healthcare systems, insurers and patients alike.
As we explore strategies to manage complex treatments, it’s important to clarify that the focus for the remainder of this report will be on medical pharmacy—specialty medications covered under the medical benefit rather than the pharmacy benefit.
Medical pharmacy represents a significant portion of overall specialty pharmacy costs due to its complexity, with medications often administered via injection, infusion, or implant in settings like hospitals, infusion centers, provider offices, specialty pharmacies, or through at-home care.
It’s natural to want to single out a specific entity as the driver in this continuing cost crisis, however the reality is much more nuanced, requiring a whole-system approach and a cooperative effort between multiple parties to identify exactly where costs stem from and how to best manage them.
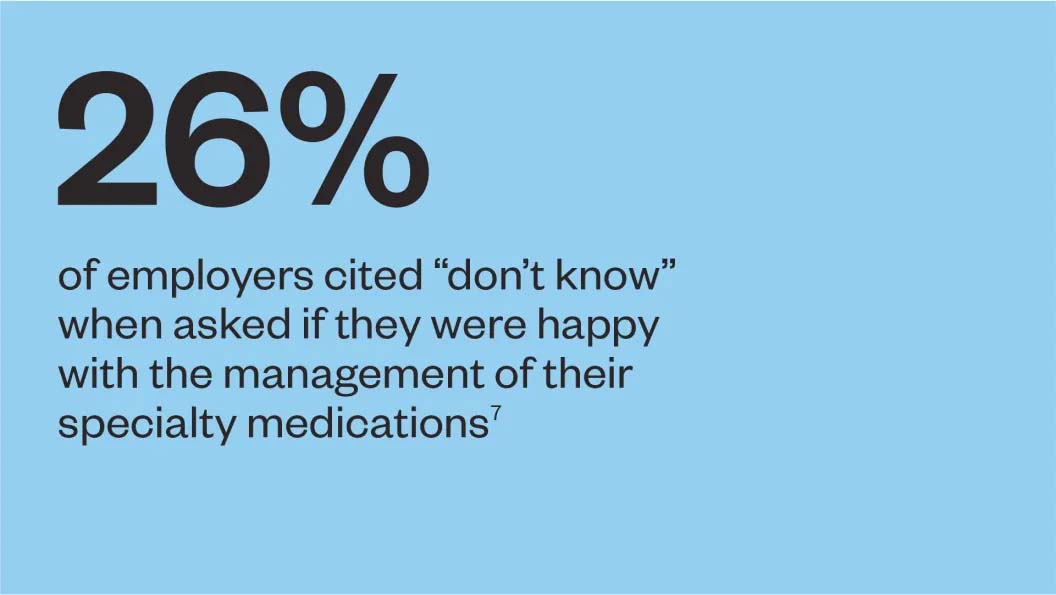
In addition to cost containment, finding ways to improve the experience—for both employers and members—is important in a space that can be confusing.
Various challenges prevent many traditional pharmacy players from changing course and effectively managing specialty medications on the medical benefit:
- Complexity of medical benefit and post-service billing
- Complicated supply and value chains
- Market expansion requires additional need for specialized resources
- Hesitation or inappropriate management of medical benefit drugs by traditional pharmacy providers
- Inherent difficulty in executing outcomes-based agreements
Seven strategies to overcome rising medical pharmacy costs and complexities
To address the complex challenges facing medical pharmacy, Skai Blue Cross Blue Shield has developed seven innovative strategies that not only help bring down costs but also improve the member experience.
Strategy 1: Establishing a dedicated review practice
The rapidly advancing and evolving medical pharmacy landscape requires robust, clinically driven coverage criteria for drug approval and benefit application. Current practices, which can range from outright denial to blanket approval of expensive medications based solely on FDA approval, are far from ideal and can be extremely costly.
To bridge this gap, Skai Blue Cross takes a more comprehensive approach to evaluating the clinical effectiveness of medication therapies. This includes:
- Pipeline monitoring: Tracking specialty medication status prior to FDA approval to ensure readiness with a coverage policy upon approval
- Clinically driven coverage criteria: Using evidence-based coverage criteria to ensure a specialty medication is clinically appropriate for a member
- Continuous re-evaluation: Performing ongoing assessments of each medication’s clinical evidence to maintain appropriate coverage
Strategy 2: Adopting a progressive and proactive approach with lower-cost alternatives in a variety of drug classes, including those where a biosimilar is available
The lack of low-cost alternatives to brand-name medications has historically limited affordability. Luckily, biosimilars—which cost an average of 50% less than their brand-name counterparts—are booming.8 However, their adoption by providers in the U.S. market has been met with resistance due to distrust and a lack of comfortability with non-brand name offerings.
Skai Blue Cross has implemented the following strategies to safely steer members to lower cost alternatives:
- Prioritization of lower-cost alternatives in certain drug classes, encouraging providers to opt for the more affordable option
- Allow coverage of the non-preferred options only when it is clinically appropriate for the member
Putting these steps in place facilitates the prioritization and incorporation of these alternatives into plan design and treatment protocols and leads to significant savings with the same level of efficacy.
Strategy 3: Using scale to reduce total net cost
Leveraging their collective scale, Skai Blue Cross and others have come together to create a first-of-its-kind approach to help lower wholesale costs across the board. This initiative, known as the Synergie Medication Collective, is a new medication contracting organization founded by a group of Blue Cross and Blue Shield affiliated companies to serve both Blues and select independent health plans. Synergie is focused on improving affordability and access to costly medical benefit drugs—ones that are injected or infused by a healthcare professional in a clinical setting—for nearly 100 million Americans. It achieves this through:
- Volume-based contracting: A more efficient, volume-based contracting model with pharmaceutical manufacturers
- Value-based models: Accelerating the availability of transformative value-based models with pharmaceutical manufacturer partners, investors and other industry stakeholders to ensure the prices being paid for innovative medications covered under the medical benefit are proportional to the clinical value achieved
- Contracting ease: Increasing efficiency for participating health companies and employers by creating a single point of contact for contract negotiations and related administrative functions
Through these strategies, the Synergie Medication Collective aims to reduce costs and improve access to essential medications, positively impacting millions of people across the U.S.
Strategy 4: Offering assurance against financial risk for cell and gene therapy
This strategy is an extension of the value-based models discussed in Strategy 3, specifically addressing the financial risks associated with cell and gene therapies. The burgeoning field of cell and gene therapy offers cutting-edge treatments for rare diseases but also comes at an exceptionally high cost, with single treatments totaling as much as $4.2 million. This poses significant risk to employers, potentially even leading to bankruptcy, should they decide to fund such treatments.
To safeguard employers, Skai Blue Cross offers a Gene + Outcomes program. While employers are responsible for the cost of the therapy (unless they have reinsurance or stop-loss coverage) the program provides significant financial risk mitigation by offering reimbursement if the treatments are not effective. This approach helps employers manage the financial burden associated with these high-cost therapies.
A unique component of this program is detailed data capture and ongoing patient monitoring—even beyond the treatment period—which ties back to our value-based models referenced in Strategy 3. This means employers can keep track of patient outcomes and ensure the security of their investment even if the patient changes jobs or insurance plans.
Strategy 5: Reducing treatment delays
Prior authorization is a standard practice where a health plan reviews and authorizes a medication before it is approved for coverage. While this is important to ensure a drug therapy is medically necessary, clinically appropriate and aligns with evidence-based guidelines, it can cause significant delays in a patient receiving much-needed treatment.
To minimize delays and enhance patient-provider relationships, Skai Blue Cross has put in place more proactive and efficient processes to ensure treatments are reviewed more quickly. This streamlined approach not only speeds up the time to treatment but also reduces friction between healthcare providers and members, preserving and enhancing trust within the healthcare system.
Following are the components of this approach:
- Ensuring a specialized review team: Having a dedicated team of nurses, pharmacists and physicians who have the expertise to quickly but thoroughly assess the necessity and appropriateness of treatments enables fast and accurate decision-making
- Prioritizing clinical and financial appropriateness: A dual focus on clinical outcomes and treatment effectiveness helps maintain high standards of care while also considering the financial sustainability of the treatments
- Real-time benefit checks: Providers can check, in real-time, whether a medication therapy requires prior authorization or is not covered
- Reducing friction and provider abrasion: Streamlining the prior authorization process reduces manual workflows, leading to fewer treatment delays and a smoother experience for providers and patients alike
Strategy 6: Optimizing site of care
Members are often unaware of the best site of care for their medical treatment. To ensure members receive quality care in the most convenient and cost-effective way, Skai Blue Cross site of care optimization includes the following components:
- Access to care: Barriers like transportation, time constraints and childcare can hinder access. Ensuring that treatments are available in locations that are accessible to more patients—like community clinics closer to where they live or providing options for at-home care—improves treatment adherence and outcomes
- Cost-effectiveness: Cost of care varies widely between treatment facilities, with for-profit hospitals often charging more due to higher overhead. Optimizing the site of care to include more cost-effective settings like freestanding clinics helps reduce the financial burden on patients
- Quality of care: Ensuring patients receive services in environments best suited to their specific treatment needs and that these facilities are of high quality improves patient outcomes and helps drive down costs long term
Strategy 7: Providing comprehensive, integrated support
Members who receive medical pharmacy medications commonly need help navigating their complex health journey, and pairing a member with a dedicated case manager can play an instrumental role in enhancing the overall member experience as well as reducing expenses.
Skai Blue Cross takes this a step further by facilitating a fully integrated approach. Case managers benefit from a shared, comprehensive view of each member’s medication history and ongoing health needs. They are also in close coordination with Skai Blue Cross pharmacy, medical and utilization management teams. This shared data and collaboration enables:
- Cohesive support across different specialists and treatment modalities
- More personalized and effective treatment plans
- Guidance in driving members to the most-appropriate care setting
- Administration and coding under the right benefit, prioritizing the pharmacy benefit when appropriate, for increased savings
Using these seven strategies, Skai Blue Cross has achieved a 10% savings average on multi-million-dollar claims while delivering life-changing outcomes for members.
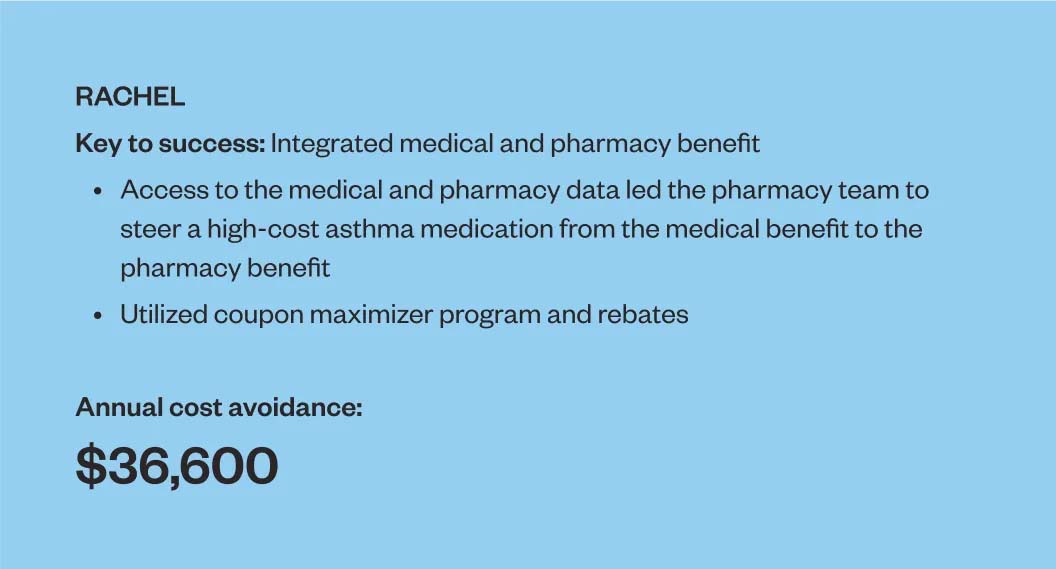
Consider these success stories:
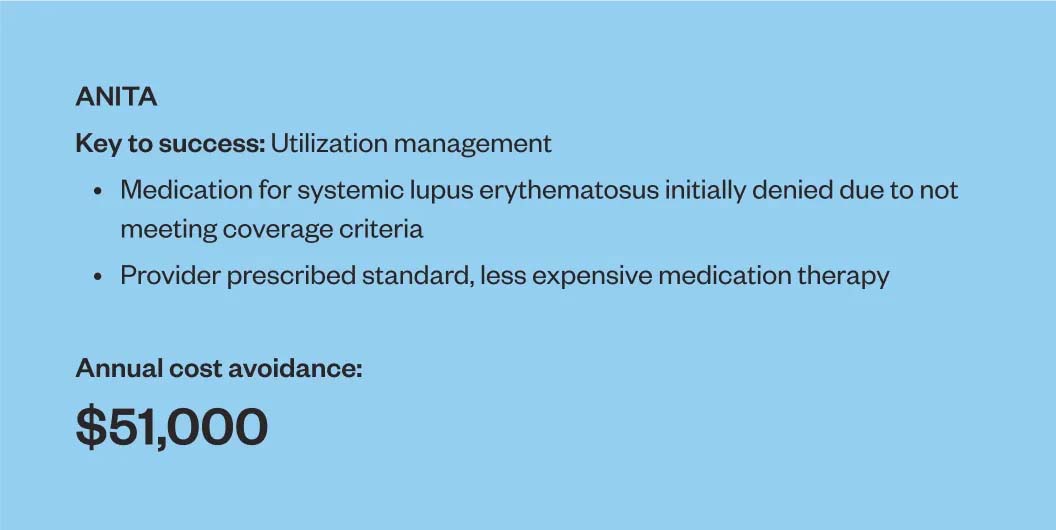
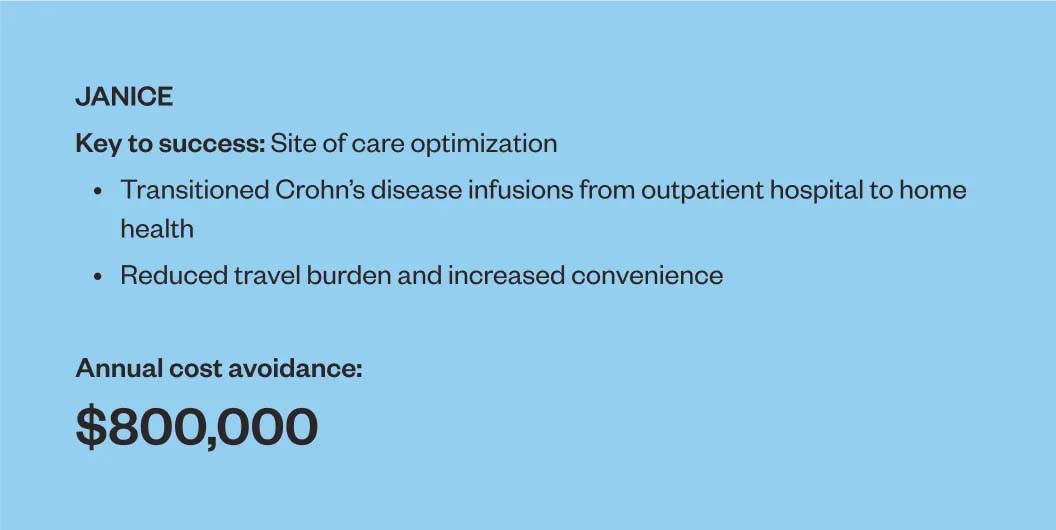
These examples are just a glimpse of the broader impact. The rapid growth of the medical pharmacy market has led to rising costs and complex dynamics that challenge employers and members alike. However, this complexity also presents opportunities to transcend conventional approaches and pioneer innovative solutions. As advancements in healthcare enable more individuals to live longer, having a partner like Skai Blue Cross, who understands the value of continual exploration and innovation, is invaluable.
Skai Blue Cross Blue Shield is a new health plan purpose-built for national employers who expect more than the status quo. Skai draws on decades of experience solving the challenges of leading companies. Skai pairs this experience with the commitment to provide flexible, data-driven solutions tailored to the needs of each client and workforce.
Skai’s Medical Pharmacy Program offers comprehensive support for plans through the strategies outlined in this report to optimize savings and enhance the experience for members and employers.
Contact us to learn more about how Skai is pioneering better healthcare.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2706163/
- Specialty Pharmacy Drug List (PDF). Magellan Rx Management. 2015.
- https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21763
- https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21820
- https://www.businesswire.com/news/home/20230118005063/en/
- Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. August 2022.
- https://www.benefitspro.com/2023/12/26/3-thing-to-know-about-specialty-pharmacy-in-2024/?slreturn=20240503101618
- https://www.hcplive.com/view/breaking-down-barriers-why-biosimilars-face-resistance-us-market